What is lymphoma?
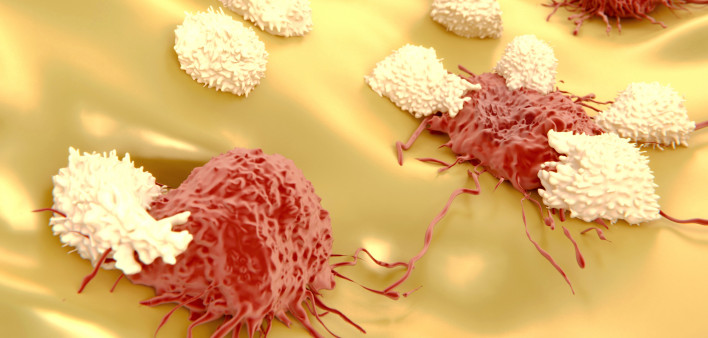
Lymphoma occurs when white blood cells of the immune system grow out of control. It can involve B cells, T cells or natural killer cells, three kinds of lymphocytes. There are two main types, Hodgkin lymphoma and non-Hodgkin lymphoma, each of which has multiple subtypes. Lymphoma can often be put into remission and in many cases can be cured, but untreated, fast-growing lymphoma can be life-threatening.
Lymphoma begins in the lymphatic system—a network of lymph vessels and organs that play a role in immune function and waste removal—but it can spread throughout the body, a process known as metastasis. It may arise in lymph nodes, bone marrow (the spongy tissue inside bones that produces blood cells), the tonsils (immune organs at the back of the throat), the thymus (an organ in the chest where T cells develop), the spleen (an organ near the stomach that stores and recycles blood cells) or lymph tissue in the stomach and intestines.
What are the types of lymphoma?
In Hodgkin lymphoma, large abnormal lymphocytes (usually B cells) called Reed-Sternberg cells build up in the lymph nodes. Most people in developed countries have what is known as the classic type. It typically starts in lymph nodes in the chest, armpits or neck. It may spread through lymph vessels to other lymph nodes, but it usually does not spread elsewhere in the body. It generally responds well to treatment and can often be cured.
Non-Hodgkin lymphoma (NHL) usually involves B cells, but T cells may also be affected. NHL may be either aggressive (fast-growing) or indolent (slow-growing). It is further classified according to the type of lymphocyte involved, how the cells look and their biomarkers or genetic characteristics.
Diffuse large B-cell lymphoma (DLBCL) is the most common type of aggressive NHL in the United States, making up nearly a third of all lymphoma cases. A subset of DLBCL, primary mediastinal B-cell lymphoma, starts in the chest and mainly affects young women. DLBCL requires prompt treatment because it grows rapidly, but response is generally good.
Burkitt lymphoma is more common in children than in adults. There are two varieties. The type seen in the United States often starts in the abdomen and can spread to the brain and spinal cord. A different type seen in Africa, linked to Epstein-Barr virus, often starts in facial bones like the jaw.
Mantle cell lymphoma, making up about 5 percent of lymphomas, has an intermediate growth rate and does not respond as well to treatment.
Follicular lymphoma is the most common indolent type of B-cell NHL, accounting for about 20 percent of lymphoma cases. It grows slowly but is hard to cure and sometimes can evolve into DLBCL.
Small lymphocytic lymphoma is similar to chronic lymphocytic leukemia, but the abnormal cells are more likely to be found in the lymph nodes rather than the blood and bone marrow.
Marginal zone B-cell lymphomas usually do not spread from where they originate. One subtype, mucosa-associated lymphoid tissue, or MALT lymphoma, usually starts in the stomach and is linked to bacteria that cause stomach ulcers.
Primary central nervous system lymphoma is an uncommon type of B-cell NHL that starts in the brain or spinal cord. It is more common in older people and those with weakened immune systems.
There are many types of T-cell lymphoma, most of which are uncommon. Precursor T-lymphoblastic lymphoma is similar to acute lymphoblastic leukemia, arising from lymphocyte precursor cells. Peripheral lymphomas involve more mature T cells.
Mycosis fungoides, Sézary syndrome and primary cutaneous anaplastic large cell lymphoma are T-cell lymphomas of the skin. Some B-cell lymphomas also primarily affect the skin.
Who gets lymphoma?
About 8,300 people develop Hodgkin lymphoma and about 1,000 people will die from it annually in the United States, according to the American Cancer Society. It is most likely to occur among teens and young adults, but the risk rises again after age 50.
About 72,200 people develop non-Hodgkin lymphoma and about 20,100 people die from it annually in the United States. A majority of people who develop NHL are over 65, and it is more common in men than in women. More than 80 percent of people with NHL in the United States have B cell lymphomas, but the distribution of lymphoma types differs around the world.
Together, Hodgkin lymphoma and non-Hodgkin lymphoma account for about 8 percent of childhood cancers, each with about 800 children and teens diagnosed annually. Boys are two to three times more likely to develop lymphoma than girls.
What are the risk factors for lymphoma?
Risk factors for lymphoma include family history, exposure to radiation and possibly exposure to some drugs and chemicals. People with HIV and those taking immune-suppressing drugs are at higher risk for lymphoma, as are those with certain autoimmune diseases.
Epstein-Barr virus (a virus in the herpes family), human T-cell lymphotropic virus 1 (HTLV-1) and human herpes virus 8 (HHV-8) can directly cause some types of lymphoma, and the risk also rises with chronic infections like hepatitis C that cause ongoing immune activation.
What are the symptoms of lymphoma?
Many people with lymphoma do not have symptoms during the early stages of disease. Later symptoms depend on where the cancer is growing, for example in the abdomen, chest or brain. As the cancer progresses, symptoms may include:
- Swollen lymph nodes
- Fever, chills and night sweats
- Frequent infections
- Fatigue
- Loss of appetite or unexplained weight loss
- Unexplained cough or shortness of breath
- Swelling or feeling of fullness in the abdomen
- Cognitive changes
- Skin rash or red, itchy patches on the skin
- Nodules or bumps under the skin
Swollen lymph nodes related to lymphoma are usually not painful, while those that swell because of an infection are often sensitive to the touch.
How is lymphoma diagnosed?
Early detection and treatment of cancer increases the likelihood of good outcomes. The process of diagnosis starts with a physical exam and health history, including how long symptoms have been present.
A blood test known as a complete blood count takes an inventory of the different types of blood cells. A sample of lymph node tissue (a biopsy) or entire lymph nodes may be removed and examined under a microscope. In some cases, a bone marrow biopsy may be done. Cells are tested for biomarkers and genetic mutations to help determine the type of lymphoma and its potential treatment. Other imaging tests, including X-rays, ultrasound, computed tomography (CT) or MRI scans may be done to see how much the cancer has spread.
How is lymphoma treated?
Treatment for lymphoma varies according to the type of disease, how how the cancer has spread, and the patient’s age and previous treatment history. Cancer that did not respond to prior therapy or has relapsed is harder to treat.
Watchful waiting: Treatment may not be started right away and the patient is monitored for signs and symptoms of disease progression, known as active surveillance. This may be an option for indolent NHL.
Surgery: Some localized lymphomas (for example, lymphoma confined to the spleen) may be surgically removed.
Radiation: Radiation is used to reduce the number of abnormal white blood cells. It may be used in conjunction with other forms of treatment.
Chemotherapy: Traditional chemotherapy works by killing fast-growing cancer cells. It can also destroy rapidly dividing healthy cells, such as those in the gut or hair follicles, leading to side effects like nausea and hair loss.
Targeted therapy: Targeted drugs work against cancers with specific characteristics. For example, they may interfere with signaling pathways that regulate cell growth. Other types of targeted therapy help the immune system recognize and attack cancer cells, including antibodies that target CD20 and other proteins on B cells.
Immunotherapy: This type of treatment helps the immune system fight cancer. For example, some tumors can turn off immune responses against them, and drugs known as checkpoint inhibitors can restore T cells’ ability to recognize and destroy cancer cells. Two PD-1 checkpoint inhibitors are approved for advanced classic Hodgkin lymphoma.
CAR-T: The newest type of treatment, chimeric antigen receptor T-cell therapy, involves removing a sample of T cells, genetically reprogramming them to recognize and attack cancer cells and putting them back into the body. One of the first approved CAR-T therapies treats adults with DLBCL.
Stem cell transplant: Bone marrow contains stem cells that give rise to all types of blood cells. A patient’s cancerous blood cells are destroyed with radiation or chemotherapy and replaced with either preserved stem cells from the same individual or bone marrow from a donor. There is a risk that donor immune cells will attack the recipient’s tissues, known as graft-versus-host disease.
New types of immunotherapy, including CAR-T, were originally developed for blood cancers like lymphoma and leukemia. Some people respond very well to this kind of treatment, remaining cancer-free for years, but others do not respond as well. Many clinical trials are underway to test experimental therapies for different types of lymphoma.
Click here for a list of approved medications used to treat lymphoma.
For more information on lymphoma, visit:
American Cancer Society: Hodgkin Lymphoma
American Cancer Society: Non-Hodgkin Lymphoma in Adults
American Cancer Society: Non-Hodgkin Lymphoma in Children
American Cancer Society: Lymphoma of the Skin
Last Reviewed: November 28, 2017