An air traffic controller for more than 30 years, Eric Tandberg is used to living with stress.
He has also guided himself through years of cancer treatments, including three blood stem cell transplants at Seattle’s Fred Hutchinson Cancer Center after he was diagnosed in 2009 with multiple myeloma.
“I have volunteered for almost every clinical trial they’ve ever thrown my way,” said Tandberg, a friendly 58-year-old who still enjoys chopping wood to heat his home in Covington, Washington.
In all those years of treatment, perhaps the most unnerving experience came in January, when he had a new round of chemotherapy that led to an eerie loss of feeling in his feet and toes, interspersed with stabbing pain at the bottom of his heel.
Diagnosis: peripheral neuropathy.
Many cancer chemotherapy drugs are life savers, but they can come with side effects of damage to nerves, especially to axons — the long, thready structures that extend through our hands and feet. These are the peripheries where we feel hot and cold, pressures, pleasure and pain.
“It’s a big problem,” said Fred Hutch oncologist Gary Lyman, MD, MPH, a recently retired expert in the treatment of chemotherapy side effects. “It is primarily a quality-of-life disruptor for many patients. They are often stuck between a rock and hard place, which is treating the cancer effectively and dealing with those toxicities.”
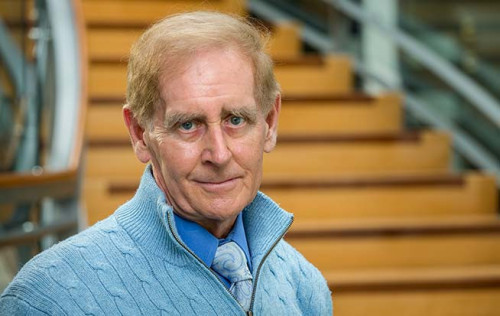
Fred Hutch physician-scientist Gary Lyman, MD, MPH, a recently retired expert in the treatment of chemotherapy side effectsCourtesy of Fred Hutch News Service
There are few precise measures of how many cancer patients deal with chemotherapy-induced peripheral neuropathy, or CIPN, but the scope of the problem is clearly enormous. Scottish researchers conducted a review of studies and concluded that 68% of cancer patients experience peripheral neuropathy in the first month after chemotherapy. That drops to 60% after three months but remains at 30% six months into treatment.
Since roughly 1 million Americans each year receive chemotherapy for the first time, these numbers suggest that 300,000 newly treated cancer patients in the U.S. are experiencing CIPN so serious that it lasts six months or more. Globally, an estimated 9.8 million people require first-course chemotherapy each year. That translates into 3 million serious cases of CIPN worldwide.
Patients like Tandberg will tell you that the condition runs a spectrum: from lack of sensation, to weird sensations of tingling, to overt and agonizing pain.
“It’s not really that you can’t feel anything,” Tandberg said of the numbness and tingling. “It’s that you can’t feel things as well as you could before.”
Of course, pain itself has a function: to warn us against hazards ranging from infection to burns to broken bones. Neuropathy can stifle that natural protection.
“I actually dropped a log on my foot about five days ago,” Tandberg said in a recent interview. “I was splitting wood and something fell off and landed on my little toe. It did hurt, but I didn’t realize how bad it hurt until a day later. I really did smash that thing.”
Since this year’s chemotherapy, his feet often feel numb; at times he feels pain at the top of his toes, in the arch of his foot, and down to the bottom of his heel. Daily activities can be uncomfortable.
“Even putting on slippers hurt. Anything that squeezed my foot even the slightest, I didn’t want them on. For a while, I wore my shoes with laces untied,” he said.
Elizabeth Loggers, MD, PhD, is medical director of Palliative Care at Fred Hutch. Cancer patients who have chemotherapy-induced peripheral neuropathy are often referred her way.
“It is a common problem. The risk of having it is increased if you have underlying medical conditions that affect the nerves such as diabetes. It is also affected by which chemotherapy you receive and how much of it,” she said.
Among the drugs mentioned most often that can cause neuropathy are taxanes, which are widely prescribed for breast cancer and gynecological malignancies as well as tumors of head and neck, stomach, lung and prostate. Up to 83% of patients taking commonly prescribed taxanes, including paclitaxel (often sold as Taxol), experience some level of peripheral neuropathy, with severe cases affecting 33% of patients, according to one study.
Also cited frequently for peripheral neuropathy side effects are platinum-based chemotherapy agents such as cisplatin, carboplatin and oxaliplatin. All are essential tools for arresting deadly tumors, but oxaliplatin, for example, is implicated in chronic neurotoxicity in 73% of patients who receive it.
“People look at peripheral neuropathy and think, ‘it’s an inconvenience,’” said Anne Marie Mercurio, a lobular breast cancer survivor living near Jacksonville, Florida, who advocates for patients. “But it’s not an inconvenience. It’s potentially life threatening.”
In 2020, Mercurio’s 83-year-old mother developed numbness in her hands and feet during treatment for metastatic breast cancer. Recovering from chemo at home alone amid the COVID-19 pandemic, she apparently rose from her chair and fell. Two relatives found her on the floor while delivering a meal. Ten days later, she died.
“The numbness in her feet must have gotten her,” Mercurio said. “How long was she lying on that floor, when nobody knew she was on that floor?”
Limited Treatment Options
Quality of life issues are key consideration for Loggers and other experts in palliative care — a term often misunderstood as applicable only to people who are dying. In fact, the goal of palliative care specialists is to relieve pain and stress at all stages of serious illness, providing comfort and support.
“Peripheral neuropathies not only can affect motor nerves and sensation, but also a person’s ability to sleep, their ability to go back to work and to interact with family and friends,” Loggers said. “It is a significant problem that, I think, is more complex and more difficult to treat than other kinds of cancer pain.”
As commonplace and impactful that peripheral neuropathy is for cancer patients, effective treatment options are limited. One approach is to treat it the same way as athletic injuries, where nerve damage is addressed, for example, through physical therapy — guided motion, balance training, stretching and muscular strengthening.
Physiatrist Hanna Hunter, MD, is Medical Director of Cancer Rehabilitation at Fred Hutch. “My clinical practice is focused on mobility and function,” she said. “My goal is to optimize their ability to be as independent as possible or engage in the activities they like to do.”
She and her team members work with patients to come up with a treatment plan, whether it is for weakness, numbness, pain or loss of dexterity. She notes that the “vast majority” of peripheral neuropathy symptoms will improve on their own after chemotherapy. That is because drugs tend to wound nerve cells, not kill them, and they have the potential to recover over time. Yet a significant subset of patients endure lingering numbness, tingling or pain.
“I advocate that patients bring up their symptoms early, because if it is due to a medication, we can mitigate it as soon as possible,” Hunter said.
Oncologists will often dial back the dosage of neurotoxic drugs once neuropathy develops. Moving quickly to treatments ranging from physical therapy to integrative approaches, such as massage, yoga and acupuncture may also help.
Terry Arnold lost much of the feeling in both her hands 15 years ago after treatment with Taxol for inflammatory breast cancer. At the time a successful seamstress, she had to abandon that work because of a near total loss of feeling in her hands.
“Who doesn’t work with their hands?” said Arnold, who lives in Sealy, Texas, west of Houston.
She became an advocate for patients like herself and founded the IBC Network Foundation. It supports research into inflammatory breast cancer — a rare, aggressive and often lethal form of the disease. Some sensation has returned to the palms of her hands, and she never lost the ability to move her fingers, grip a steering wheel, or type.
“When your hand is numb, it tingles from the inside, but you could stick a pin on the outside and I won’t know it’s there,” she said. When she fell and broke a bone in her hand, she didn’t realize she was hurt until her hand turned colors.
“I have to be careful about things I do in the kitchen, because it’s such a danger field for me,” she said. She uses her elbow to test water temperature and is extra careful about handling sharp objects.
“I am not saying stop using Taxol,” Arnold stressed. “I am grateful to be alive, so I don’t want to complain about these side effects. But it has altered my life.”
Cancer patient Tandberg’s experience with peripheral neuropathy is very recent, and to address it he was prescribed acupuncture, the East Asian medical practice of inserting needles into the skin at key point across the body.
Even though his neuropathy is confined mostly to his feet and toes, he signed up for eight weeks of acupuncture treatments at Fred Hutch that involve placement of needles on his feet, his hands and on his forehead, just above the bridge of his nose.
His acupuncturist, who manages the Fred Hutch Integrative Medicine program, is Jonathan Siman, DACM, LAc — a licensed acupuncturist with a Doctorate in Acupuncture & Chinese Medicine.
“Many of our patients who have finished their course of chemotherapy have lingering, chemo-induced neuropathies,” Siman said. “The main complaints are numbness, tingling and pain, and some patients also have heat and cold sensitivity.”
Tandberg said that after several sessions on the acupuncture table, during which he also took duloxetine, a drug used to treat diabetic neuropathy, he experienced a gradual reduction in numbness and foot pain. He describes it as a dialing down, rather than a switching off of his symptoms. It has turned a disturbing and sometimes painful condition into a “tolerable annoyance.”
“My feet are still numb, but not as bad,” he said. “I can grab my toes and feel it. After three or four weeks with Jonathan, I could bend my toes again. That was awesome.”
Siman notes there is a growing body of evidence supporting the use of acupuncture to manage CIPN symptoms. However, he said larger, rigorous trials are needed to support the use of acupuncture for this condition.
There is a subjective element in treating pain, as well as in measuring the effectiveness of pain management strategies, including complementary medical treatments such as massage, yoga or acupuncture. Measuring pain relies on patient reporting of their experience, such as how they would rate their pain on a 10-point scale.
A Fred Hutch Clinical Trial of Acupuncture
Siman is co-investigator on a Fred Hutch clinical trial, led by oncologist Stacey Cohen, MD, which is currently enrolling up to 56 patients with gastrointestinal cancer. The investigators are testing the effectiveness of acupuncture and acupressure (a needle-free use of pressure or massage on certain acupuncture points) in combination with today’s standard of care, cryotherapy, the application of cold or ice to the mouth, hands or feet. Some patients will be assigned 12 weeks of acupuncture and self-administered acupressure plus cryotherapy; others will just get cryotherapy alone.
Trials like this one can build on that evidence and either strengthen or weaken the case for using acupuncture in specific clinical situations, depending on the findings.
Siman said it is true that the mechanism of action explaining why acupuncture works “is not yet fully understood.” Some studies have shown that acupuncture reduces inflammation and improves blood flow to repair damaged nerves. Another working hypothesis is that it stimulates natural pain-reducing chemicals — endorphins and enkephalins — produced in the brain.
“The potential for harm is low here, and early studies have shown some benefits, but we don’t have the evidence base to say, ‘yes, everybody should be getting this to prevent or treat neuropathy,’’’ Siman said. “However, we do know that peripheral neuropathy is a hard thing to manage, and having additional tools is great for patients, so we obviously want to find out more from these studies.”
Heather Greenlee, ND, PhD, is medical director of the Integrative Medicine Program at Fred Hutch, which offers acupuncture, mind-body approaches and counseling on the appropriate and safe use of dietary supplements to alleviate symptoms of cancer patients and promote their overall well-being.
“Chemotherapy-induced peripheral neuropathy dramatically effects quality of life for many of our patients,” said Greenlee, who is senior investigator for the acupuncture trial. “For some people, peripheral neuropathy or the risk of CIPN alters the course of their cancer treatment. We’ve had patients who are surgeons or musicians or pilots — people who definitely need control of their hands — or athletes who need to be able to use their feet.
“We don’t have a good way to predict who will and will not develop CIPN. We are working on studies to prevent CIPN from happening, looking a risk factors for it, and looking at how to treat it once it develops,” she said.
Meanwhile, Greenlee and her team are also investigating the use of acupuncture to decrease opioid use in patients receiving bone marrow transplants and to decrease common side effects of bladder cancer treatment.
In previous research at Columbia University, she worked on a study testing whether acetyl-carnitine, a dietary supplement used in HIV and diabetes to reduce peripheral neuropathy, might help breast cancer patients. “Instead, it made it worse,” she said. “This is why we need to do research. Just because it’s natural, or integrative medicine, doesn’t mean it’s safe or benevolent all the time. We need to test it.”
Greenlee co-chairs the Clinical Practice Guidelines Committee of the Society for Integrative Oncology, and she works closely with Lyman on developing guidelines for SIO and the American Society of Clinical Oncology on the use of integrative therapies to manage different symptoms and side effects frequently experienced by people with cancer. Although Lyman has retired, he remains an affiliate investigator at Fred Hutch and works actively on multiple projects and mentorships.
An ASCO guideline update published in 2020 reviewing approaches — both conventional and integrative — for the treatment of chemotherapy-induced peripheral neuropathy was not encouraging.
“The identified data reconfirmed that no agents are recommended for the prevention of CIPN,” the authors wrote in their abstract. Consistently, interventions evaluated for prevention or treatment were given low grades for benefits; and strength-of-evidence was similarly rated low, especially for unconventional or non-pharmacological approaches including acupuncture, cannabinoids (marijuana derivatives), cryotherapy and exercise.
Supplements and drugs fared no better. Only duloxetine, the diabetic nerve pain drug prescribed to Tandberg along with acupuncture, was supported for treating patients “with established and painful CIPN.”
Greenlee is nevertheless hopeful that scientific studies will be able to establish clearly which techniques are most effective.
“The evidence quality is still low, and the strength of the recommendations is still weak, but that is largely driven by the fact that we are early in the process of conducting trials in this area,” she said.
Unquestionably, thousands of patients are hungering for treatments for peripheral neuropathy, and evidence shows they are seeking out such remedies in spite of a shortage of definitive studies. At Fred Hutch alone, the Integrative Medicine program, with four licensed acupuncturists on staff, has a three-month waiting list.
Complex, Cancer-Related Pain
Pain in cancer is by no means limited to that caused by chemotherapy. Nerves can be damaged by cancer-related compression fractures and direct pressure from tumor growth. Fred Hutch has organized teams of caregivers who focus on it. Lauren Holtz, clinical nurse coordinator for the Pain and Palliative Care clinics, said these groups specialize in “complex, cancer-related pain.”
Those conditions frequently involve severe aches and stabbing pains, either chronic or acute, and may require treatment with analgesics — including opiates.
“At the pain clinic, we are not necessarily treating peripheral neuropathy unless it gets to the point where it is painful,” Holtz said. If the condition is primarily numbness or lack of sensation, the patient may be referred to the palliative care clinic, to integrative medicine, or to physical therapy for appropriate care.
Experts like Lyman agree that more attention needs to be paid to peripheral neuropathy, either caused by cancer itself or the side effects of treatment. Though retired, he continues to work on developing for ASCO updated guidelines for treatment and prevention of CIPN. Lyman said it’s important for oncologists to be trained at the outset of their careers to be alert to it, and to make sure their patients take it seriously.
“It’s often something that the patient notices but may dismiss or think it is just something to be expected,” he said. “Detecting this early is one of the keys to minimizing the problem. The earlier it is addressed, the more likely it will reverse, or at least not progress to really debilitating symptoms.”
This article was originally published March 27, 2023, by Fred Hutch News Service. It is republished with permission.







Comments
Comments