Why do some people hospitalized with COVID-19 succumb, while others—with apparently similar disease severity at the time of hospitalization—survive? Among older individuals, are there particular immune responses to SARS-CoV-2 virus infection that set the stage for the increased risk of severe COVID-19?
These are among the questions addressed in the NIAID-funded Immunophenotyping Assessment in a COVID-19 Cohort (IMPACC) study. Two recent publications by IMPACC network investigators provide a detailed picture of the immunologic dynamics of COVID-19 disease in a large cohort of patients who were hospitalized prior to the wide-spread availability of COVID vaccines.
A report by Leying Guan, PhD, of Yale School of Public Health and colleagues in the Journal of Clinical Investigation describes data from this longitudinal study of 1,152 adult COVID-19 patients who were hospitalized between May 2020 and March 2021. Participants were assigned to one of five disease trajectory groups (TG) based on factors including length of hospital stay until discharge or death. Individuals in both TG4 and TG5 were considered critically ill, with those in TG5 dying within 28 days of hospitalization.
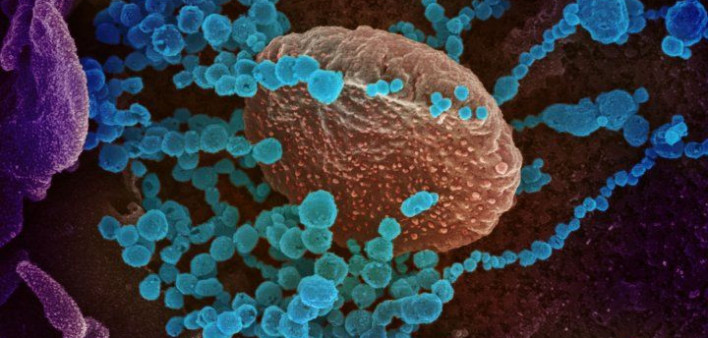
Blood and nasal swab samples, collected up to six times for each patient, underwent an integrated series of “omics” analyses. This allowed the investigators to track coordinated changes in relevant phenomena including gene expression, the appearance of various immune response proteins and metabolites, and frequency of certain effector immune cells (T cells) as well as antibody-producing B cells over the course of illness. The multi-omics analysis identified a “severity factor” that predicted seriousness of illness among all participants and another distinct immune signature, termed a “mortality factor,” that distinguished those in the critically ill groups who survived (TG4) from those who died (TG5).
The “severity factor” comprised a spectrum of immune changes that began early in the course of illness and included dysregulation in the metabolism of three essential amino acids (tryptophan, phenylalanine, and histidine). These amino acids, note the investigators, act as important protein building blocks, critical sources of energy, and modulators of immunity, and so disturbances in their metabolism could signal an increased likelihood of severe illness or death. The metabolic dysregulation revealed by the analysis demonstrated the greatest power at distinguishing TG4 from TG5 and appears to act as an early hallmark of eventual mortality among critically ill patients. These observations regarding dysregulation of amino acid metabolism suggest that methods to assess metabolites in the clinical setting early in the course of disease might prompt trials of interventions such as amino acid supplementation in those cases where a signal of dysregulation is detected.
The “mortality factor” was driven by immune system disturbances and included elevated levels of inflammation-promoting molecules called cytokines, reduced levels of infection-fighting immunoglobulins and antibody-producing B cells, and a dysregulation in the body’s responsiveness to interferon. These observations support the early administration of antiviral and antibody therapies as critical interventions to reduce COVID-19 mortality.
Charles R. Langelier, MD, PhD, of University of California, San Francisco, and colleagues recently published another analysis of data from the IMPACC cohort in Science Translational Medicine. This analysis sought to better characterize the association between increased age and greater odds of severe or fatal COVID-19 disease. Blood and nasal swab samples from 1,031 IMPACC participants were collected up to six times from each patient over a span of 28 days, yielding 2,523 samples for analysis.
In general, the investigators note, an effective response to a viral infection involves a well- controlled series of immune reactions, beginning with proinflammatory and other responses from innate immune components, followed by a regulated response from antibodies and other components of the adaptive immune system leading to viral clearance, and then a diminishment of inflammatory signals so that unnecessary tissue damage is avoided.
Compared to people under 63 years of age, those who were older had higher respiratory viral loads at hospital admission, produced lower amounts of anti-SARS-CoV-2 antibodies over time, and cleared the virus more slowly. Older age was strongly associated with increased expression of genes involved in several innate immune-related pathways, including ones leading to increased abundance of proinflammatory interferons, and these remained high over time, suggesting an age-dependent impairment in inflammation resolution.
In summary, these analyses demonstrate the value of collecting and analyzing comprehensive longitudinal immunologic assays combined with careful clinical phenotyping to identify mechanisms of disease heterogeneity in both novel and infectious diseases, an approach that may allow the identification of potential novel therapeutic targets.
References:
JP Gygi et al. Integrated longitudinal multi-omics study identifies immune programs associated with acute COVID-19 severity and mortality. Journal of Clinical Investigation. DOI: 10.1172/JCI176640 (2024).
H Van Phan et al. Host-microbe multi-omic profiling reveals age-dependent immune dysregulation associated with COVID-19 immunopathology. Science Translational Medicine. DOI: 10.1126/scitranslmed.adj5154. (2024).
This NIAID News blog post was published by the National Institute of Allergy and Infectious Diseases on May 1, 2024.






Comments
Comments